July 2025 | By Brandon Redman, VP of Healthcare Solutions
Key takeaways for payviders:
- Payviders are under growing pressure from rising healthcare costs, strained rural health systems, and instability across government-sponsored markets — making operational efficiency more critical than ever to ensure seamless member care.
- Balancing care delivery with insurance operations requires flexible automation, integrated systems, and real-time data sharing to avoid friction and reduce administrative burden.
- Automation, AI, and Master Data Management (MDM) helps payviders streamline enrollment, manage transitions between Medicaid, ACA, and Medicare, and deliver a seamless member experience.
- Diversifying coverage models and reducing payer-side admin costs can help payviders stabilize revenue, build long-term resilience, and invest in initiatives that enhance member experience and improve health outcomes.
Payviders — or provider-sponsored organizations (PSO) — have a huge opportunity to improve healthcare access and outcomes in their communities. Their dual role of delivering care and managing coverage unlocks the potential for coordinated, patient-centered coverage and support — but it also adds complexity. From enrollment to billing to member communications, things can easily fall through the cracks.
As payviders operate across Medicaid, the ACA, and Medicare Advantage, they’re facing more pressure than ever. Rising healthcare costs, mounting strain on rural health systems, and increasing premium rates for Qualified Health Plans (QHPs) are compounding financial challenges for organizations already balancing two demanding roles. The next few years are expected to bring turbulence across all government-sponsored markets — from shifting regulatory requirements to potential funding changes — and payviders will need to navigate this uncertainty without compromising care delivery or operational stability.
To withstand the pressure and deliver better member experiences, payviders must focus on two strategic priorities:
- Diversifying into new and innovative coverage models to establish additional lines of revenue, help spread financial risk across business units, and invest in initiatives that enhance member experience and improve health outcomes.
- Reducing administrative costs on the payer side by eliminating manual workflows, streamlining core operations, and leveraging automation, AI, and MDM to minimize friction and maximize efficiency, ultimately leading to better member experiences and higher satisfaction.
It’s a difficult balance — but with the right automation strategy, it’s possible to protect margins, support mission-driven care, and build a more resilient infrastructure for the future. Better operations can move the industry closer to the Triple Aim of better experience, for more of the population, at a lower per-capita cost.
The Payvider Challenge: One Mission, Two Systems
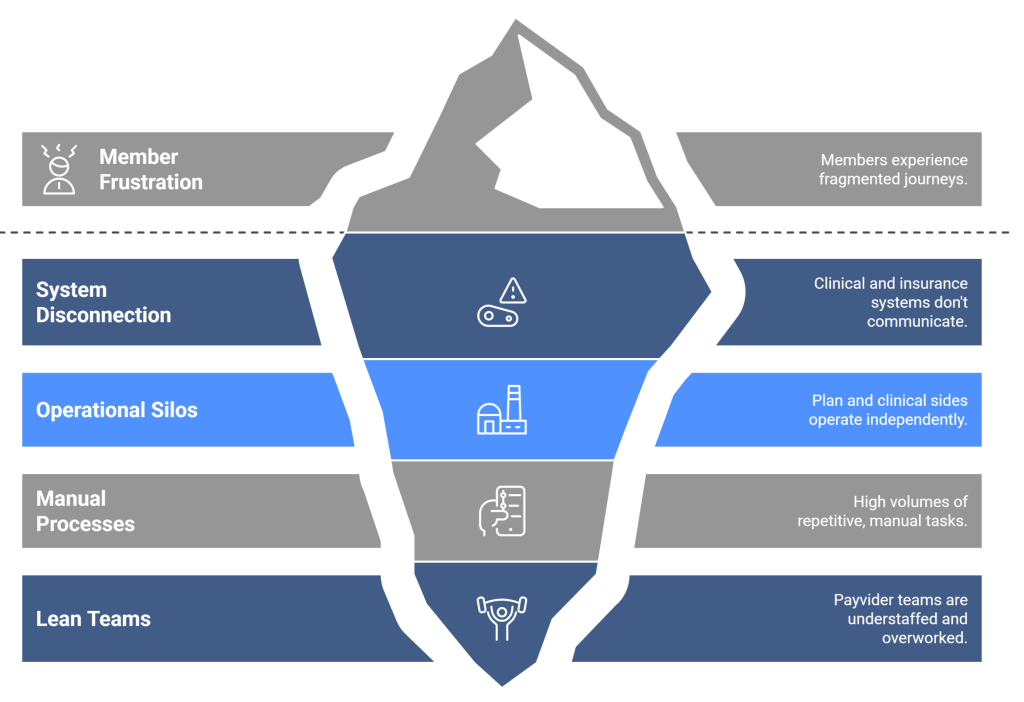
Payviders face many of the same operational pressures as traditional health plans — but with added layers of complexity tied to their provider roots. To deliver better member experiences, payviders must address these challenges head-on:
- Lean teams, heavy lifts
Payvider teams are masters of doing more with less. They run leaner than traditional payers, yet they’re responsible for more, including tasks related to both clinical touchpoints and insurance operations. They juggle high volumes of repetitive work — eligibility checks, invoice processing, manual data entry, and more. Without automation, these tasks delay approvals, slow workflows, and drain staff capacity.
- Disconnected systems, disjointed decisions
Many payviders rely on legacy systems built for either clinical care or payer operations — but not both. Information silos make administrative burdens heavier, contribute to errors, and limit the plan’s ability to anticipate its members’ needs and resolve issues. In addition, the plan side and the clinical side of payviders often operate with different financial incentives. Hospitals operating under a fee-for-service model generate their revenue through clinical visits, while health plans benefit financially from fewer visits.
- Fragmented journeys, frustrated members
Members expect a personalized experience that mirrors the care they receive as patients. But when clinical and insurance systems don’t communicate, the experience breaks down. For example, a referral might be approved on the care side but delayed on the coverage side. The disconnect can lead to confusion, treatment delays, and lost trust.
Add in the complexities of moving between Medicaid, Marketplace, and Medicare Advantage — each with different eligibility rules, plan designs, and record-keeping — and the risk of confusion or coverage gaps rises fast.
Payvider Challenges: Unveiling the Hidden Depths
Making Automation Work for Payviders
Automation is a practical way for payviders to reduce the strain on their teams and improve member experience. ScienceSoft estimates a mid-sized health payer can achieve 10-25% cost savings with automation across operational lines. AI-powered automation increases that total to 30-50%. By automating routine tasks, payviders can free up staff to focus on high-touch, high-value work that enhances the member experience.
But automation is only as effective as the systems it connects to. Application programming interfaces (APIs) are key. They allow enrollment platforms, provider systems, and coverage systems to exchange real-time data. This reduces the risk of duplicate outreach, delayed notices, and mismatched records. When systems are integrated, payviders can build workflows that deliver clarity for members and relief for staff.
Managing multiple lines of business on a single integrated platform reduces implementation risks, lowers administrative overhead, and avoids the cost and complexity of building separate technology stacks. By leveraging MDM as a core component of their unified data strategy, payviders can ensure that all systems and stakeholders have access to accurate, up-to-date, and consistent member data. Consolidation lowers admin overhead, reduces compliance risk, and accelerates time to market.
Once payviders commit to a unified data strategy, they can streamline operations by:
- Automating the day-to-day
Removing manual bottlenecks is one of the easiest ways to improve both the employee and member experience.
Tasks like enrollment processing, eligibility verification, and premium billing can all be automated — along with notices, plan confirmations, and payment reminders. Members experience fewer delays. Staff gain time to focus on high-value work.
UCare achieved this success after adopting Softheon’s solutions. Tasks that used to take a full month — like invoice processing — now take a day. Softheon enabled UCare to free up three full-time employees for strategic initiatives. UCare also improved the accuracy of its Advance Premium Tax Credit (APTC) reconciliations by 2.5%, leading to an increase of $2.1 million in reimbursements.
- Fixing member experiences
Fewer manual steps mean less friction for members. With automation in place, payviders can streamline enrollment, verify eligibility, and collect payment within hours — not days or weeks. Features like real-time payment confirmation and automated welcome notices reduce confusion and increase trust.
Automation also supports seamless transitions across coverage types. Whether members are moving from Medicaid to Marketplace or aging into Medicare, payviders can use automation to ensure each step — from eligibility checks to communications — happens on time and in the right order. When paired with strong master data management (MDM), payviders can maintain a single, accurate view of each member across programs. That continuity reduces duplication, minimizes errors, and ensures that transitions in coverage don’t result in gaps in care or confusing member experiences.
- Supporting members in real time
Integrated data allows payviders to personalize engagement based on real-world events. When a member has a hospitalization, receives a new diagnosis, or misses a payment, automated triggers can launch the right action — from benefits updates to care management outreach.
Prior authorization and referrals are often major points of friction for members and providers alike. Improving these processes via automation and other methods improves care continuity and aligns provider decisions with plan benefits.
With AI and real-time data, payviders can also guide members toward the right plan during onboarding. Personalized recommendations improve plan fit and increase satisfaction and retention.
- Enhancing plan design and risk management
Payviders have access to a unique data set: Clinical outcomes and insurance utilization. While information silos can make it hard to fully connect those insights, sharing and analyzing the data together can reveal where coverage design falls short — and how to fix it.
That might mean redesigning networks, adjusting copays, or expanding coverage to better meet the needs of their patient population. These changes support better outcomes and reduce long-term risk for both members and the plan.
Better data also means smarter forecasting. Plans can more accurately assess business risk, forecast cost drivers, and adjust pricing and benefit structures to stay financially sustainable while supporting better outcomes.
Payviders Improve Member Satisfaction through Automation and Unified Data

The Payvider Advantage
Most payviders are not chasing market share — instead, they strive to increase access while delivering higher quality care and a better member experience. Automation and AI won’t replace that mission — but they can support it. By removing the friction between care and coverage, payviders can grow sustainably, improve outcomes, and deliver a better experience for everyone they serve.
Interested in reducing administrative costs while delivering a seamless journey for members? Softheon brings all these functions together. Our integrated solutions consolidate enrollment, billing, payment, and member management into a single ecosystem that integrates with core administrative systems. With these connections, Payvider staff can work more efficiently. Members receive a seamless experience. And automation can do its job effectively.
If you’re interested in helping payviders outlast regulatory uncertainties while supporting members, reach out to me on LinkedIn! I’m ready to continue the conversation, and I’m always breaking down the latest news for payviders.


