Health Plan Operations
Made Simple.
Growth Made Possible
30M+ Enrollments
$20B+ Premiums Processed
1 in 3 ACA Plans Trust Softheon

Shop, Quote, Enroll, Bill, Communicate - All in One Place
Markets Served
Give your members the continuity of coverage they deserve across On-Exchange, Off-Exchange/ICHRA, Medicare Advantage, and Small Group.
Health Plans
Softheon helps health plans of all sizes streamline operations, reduce administrative costs, and grow with confidence.

Connection that Drives Success—In Any Market
Health Plans
Reduce admin costs and improve member satisfaction with AI-powered operations designed for scale.
BenTechs & Brokers
Serve clients better with streamlined quoting, enrollment, and benefits management built by brokers.
Government Agencies
Reduce fraud, waste, and abuse while ensuring compliance and expanding equitable coverage access.
All-in-One Solution for Payers
Endless Value for Health Plans, Members, and Markets
Expand into new lines of business with the operations backed by API flexibility and BPaaS expertise.
Automate shopping, enrollment, billing, and reconciliation with a platform built for scale.
Deliver frictionless digital experiences that help members choose, pay for, and keep their coverage.
Engage members with timely communications and integrated broker support that drive retention.
Stay aligned with CMS, IRS, and state regulations with confidence in a system trusted by regulators.
From ACA to ICHRA to Medicare Advantage, our platform processes millions of transactions every year.
Real Plans. Real Progress. Real-World Success
Trusted by Health Plans and Their Members Nationwide

“Softheon’s expert knowledge of the ACA marketplace coupled with their leading enrollment and billing technology has made them the perfect partner during Hometown Health’s first open enrollment period on the exchange.”
David Hansen | CEO, Hometown Health

“[Softheon has] a fantastic solution and its performance has been great… the strength of the vendor relationship isn’t whether you have problems or not, it’s how you go about solving them and those issues.”
Paul Wingle | WellSense

“Anyone in group coverage knows the prices are rising. And they are rising astronomically. Small employers are cutting it off and deciding to not offer more and more every year… With ICHRA, we now have an opportunity to use our Marketplace plans and, through ICHRA administration with Softheon, offer smaller employers a more affordable healthcare option.”
Daverick Isaac | Community First Health Plans
Insights to Move You Forward

Going from Over 10K to Nearly 1M Members
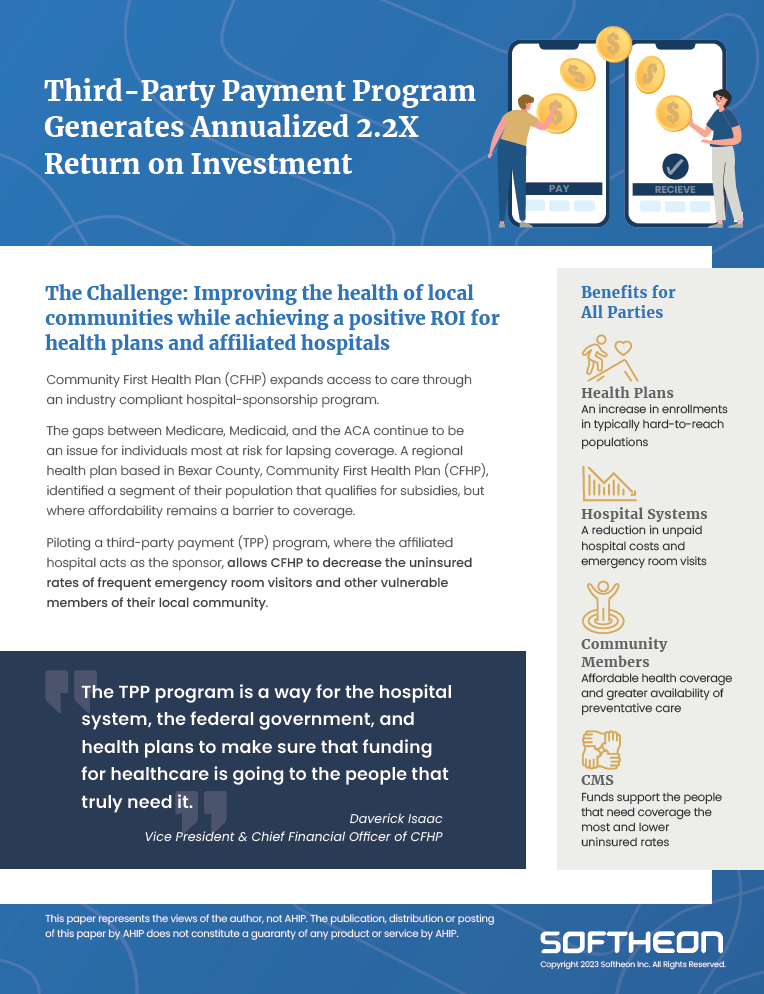
Third-Party Payment Program Generates Annualized 2.2X ROI
UCare faced significant challenges due to manual processes in shopping, enrollment, and billing, which…
Purpose-Built for the People Behind the Plans
Softheon was founded on a simple belief: healthcare should be accessible, affordable, and plentiful. For more than 25 years, we’ve partnered with health plans, brokers, and government agencies to remove barriers, reduce costs, and deliver better member experiences.
Built by the people who helped design and power the Exchanges, Softheon brings unmatched policy expertise and operational insight. And with agentic AI built into every process, we help you work smarter, faster, and more confidently. We equip the people behind the plans with technology that makes growth possible and coverage continuous.
Because when you succeed, the communities you serve thrive.

Maintain Compliance
Stay aligned with CMS, IRS, and state regulations with confidence in a system trusted by regulators.







Trusted. Proven. Compliant.
Lorem ipsum dolor
sit amet consectetur
Lorem ipsum dolor
sit amet consectetur
Lorem ipsum dolor
sit amet consectetur
Lorem ipsum dolor
sit amet consectetur
